Important Safety Information for LUPRON DEPOT-PED
What is the most important information I should know about LUPRON DEPOT-PED?
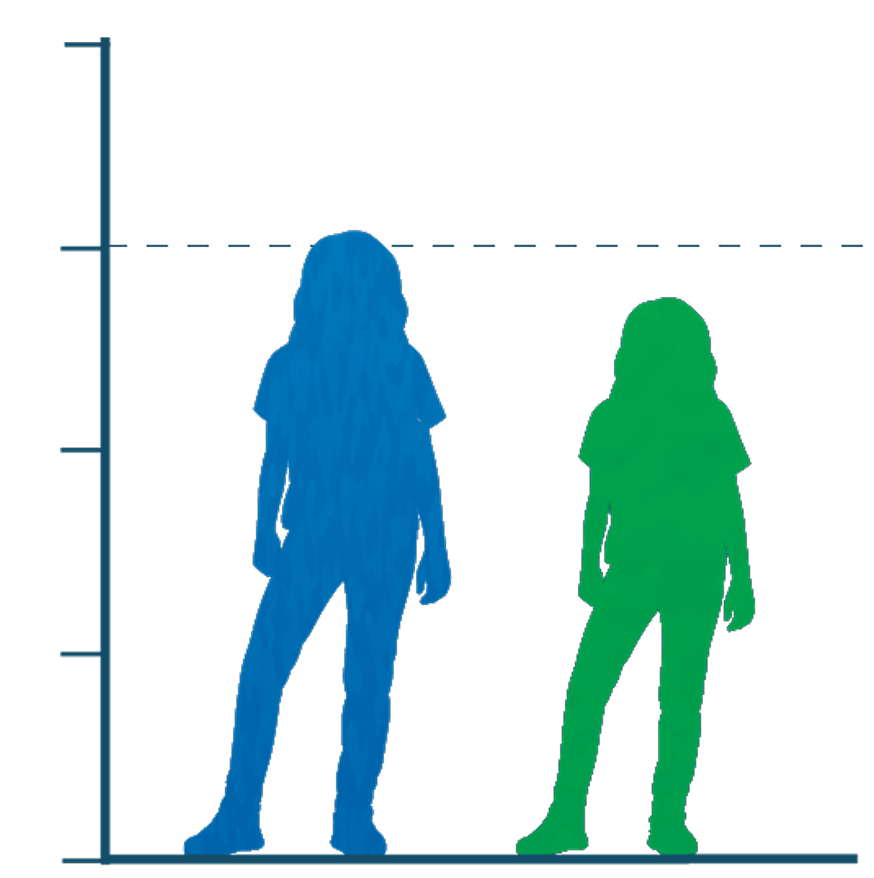
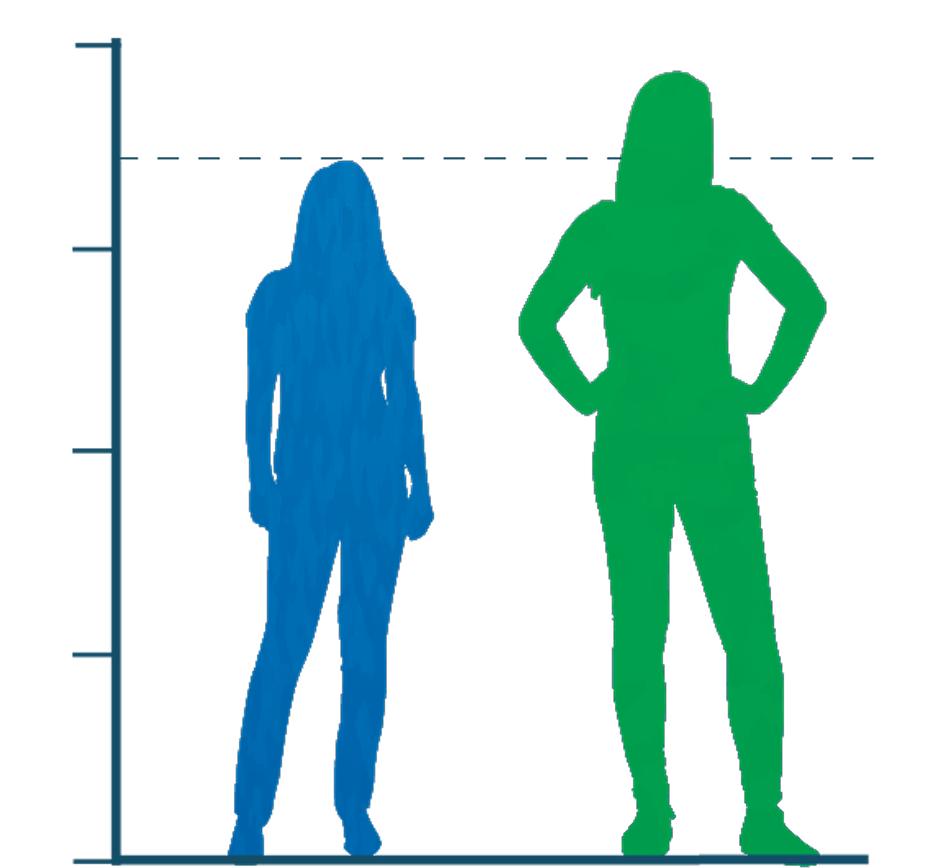
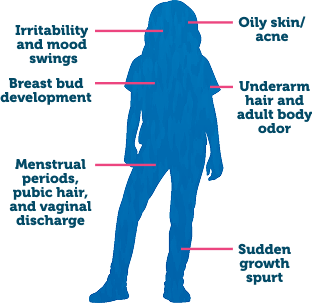
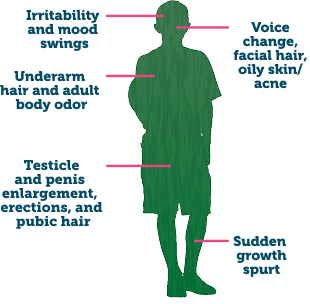
- During the first 2 to 4 weeks of treatment, LUPRON DEPOT-PED can cause an increase in some hormones. During this time, you may notice more signs of puberty in your child, including vaginal bleeding. Call your child's doctor if these signs continue after the second month of treatment with LUPRON DEPOT-PED.
- Some people taking gonadotropin-releasing hormone (GnRH) agonists like LUPRON DEPOT-PED have had new or worsened mental (psychiatric) problems. Mental (psychiatric) problems may include emotional symptoms such as:
- Crying
- Irritability
- Restlessness (impatience)
- Anger
- Acting aggressive
Call your child's doctor right away if your child has any new or worsening mental symptoms or problems while taking LUPRON DEPOT-PED.
- Some people taking GnRH agonists like LUPRON DEPOT-PED have had seizures. The risk of seizures may be higher in people who:
- Have a history of seizures
- Have a history of epilepsy
- Have a history of brain or brain vessel (cerebrovascular) problems or tumors
- Are taking a medicine that has been connected to seizures, such as bupropion or selective serotonin reuptake inhibitors (SSRIs)
Seizures have also happened in people who have not had any of these problems. Call your child’s doctor right away if your child has a seizure while taking LUPRON DEPOT-PED.
- Severe cutaneous (skin) adverse reactions may happen during treatment with GnRH agonists like LUPRON DEPOT-PED. Stop LUPRON DEPOT-PED and call your child’s doctor right away if your child has any of the following signs or symptoms during treatment with LUPRON DEPOT-PED:
- Skin rash or acne
- Dry skin
- Itching
- Blisters on your skin
- Redness or swelling of your face, hands, or soles of your feet
- Blisters or sores in your mouth
- Peeling of your skin
- Fever
- Muscle or joint aches
- Swollen glands
- Increased pressure in the fluid around the brain can happen in children taking gonadotropin-releasing hormone (GnRH) agonist medicines, including LUPRON DEPOT-PED. Call your child’s doctor right away if your child has any of the following symptoms during treatment with LUPRON DEPOT-PED:
- Headache
- Eye problems, including blurred vision, double vision, and decreased eyesight
- Eye pain
- Ringing in the ears
- Dizziness
- Nausea
LUPRON DEPOT-PED should not be taken if your child is:
- Allergic to GnRH, GnRH agonist medicines, or any ingredients in LUPRON DEPOT-PED. See the end of the Medication Guide for a complete list of ingredients in LUPRON DEPOT-PED.
- Pregnant or becomes pregnant. LUPRON DEPOT-PED can cause birth defects or loss of the baby. If your child becomes pregnant, call your child's doctor.
Before your child receives LUPRON DEPOT-PED, tell their doctor about all of your child's medical conditions, including if they:
- Have a history of mental (psychiatric) problems
- Have a history of seizures
- Have a history of epilepsy
- Have a history of brain or brain vessel (cerebrovascular) problems or tumors
- Are taking a medicine that has been connected to seizures, such as bupropion or selective serotonin reuptake inhibitors (SSRIs)
- Are breastfeeding or plan to breastfeed. It is not known if LUPRON DEPOT-PED passes into the breast milk
Tell your child's doctor about all the medicines your child takes, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How will your child receive LUPRON DEPOT-PED?
- Your child's doctor should do tests to make sure your child has CPP before treating them with LUPRON DEPOT-PED.
- LUPRON DEPOT-PED is given as a single-dose injection into your child's muscle each month, every 3 months, or every 6 months by a doctor or trained nurse. Your child's doctor will decide how often your child will receive the injection.
- Keep all scheduled visits to the doctor. If a scheduled dose is missed, your child may start having signs of puberty again. The doctor will do regular exams and blood tests to check for signs of puberty.
What are the possible side effects of LUPRON DEPOT-PED?
LUPRON DEPOT-PED may cause serious side effects. See “What is the most important information I should know about LUPRON DEPOT-PED?”
- The most common side effects of LUPRON DEPOT-PED received 1 time each month include:
- Injection site reactions such as pain, swelling, and abscess
- Weight gain
- Pain throughout body
- Headache
- Acne or red, itchy rash and white scales (seborrhea)
- Serious skin rash (erythema multiforme)
- Mood changes
- Swelling of vagina (vaginitis), vaginal bleeding, and vaginal discharge
- The most common side effects of LUPRON DEPOT-PED received every 3 months include:
- Injection site reactions such as pain and swelling
- Weight gain
- Headache
- Mood changes
These are not all the possible side effects of LUPRON DEPOT-PED. Call your child’s doctor for medical advice about side effects.